Ontario's ICU doctors have been informed to prepare for a potential triage situation due to COVID19 surging, where some patients may not receive the critical care they need.
Triage would require doctors to follow certain standards of care outlined by the Ontario COVID-19 Bioethics Table, being put in the position to ultimately decide which patients get critical care and which ones would not.
It's a scenario that made headlines in Italy early in the pandemic where hospital wards were overrun with patients, forcing doctors to prioritize intensive care for those with the best chance of therapeutic success.
The province's Critical Care COVID19 Command Centre issued a memo to ICU doctors on Wednesday, as first reported by CBC during an interview with Dr. Michael Warner of Michael Garron Hospital the next day.
The centre's incident Commander, Dr. Andrew Baker, said in a statement that given the evolving situation in Ontario, the health care system is preparing for if there is a major surge.
"The background information and tools shared are a standard way for physicians to conduct an assessment for a patient upon presentation at the emergency department or as an admitted patient requiring higher levels of care, to assess whether they should be directed to critical care," he said. "They were shared with the critical care community as background only and to ensure a common approach across the sector, so physicians and other health professional staff can learn how to quickly operationalize an emergency standard of care for admission to critical care, if ever needed."
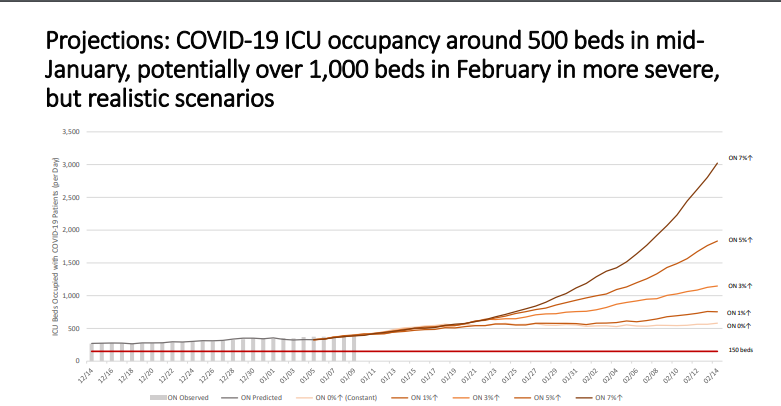
In the COVID-19 Advisory for Ontario Science Table's latest briefing on Tuesday, ICU occupancy was projected to hit around 500 beds by mid-month and potentially over 1,000 in February in "more severe, but realistic scenarios."
What concerns health officials is that current growth rates have been around three to five per cent, however some days have seen rates as high as seven per cent.
Provincial models show that consistent five per cent growth would lead to over 1,500 ICU beds by February 14th and over 3,000 requiring intensive care at seven per cent.
Currently, Ontario has about 2,000 ICU beds and projections on occupancy in both November and December became accurate.
What's exacerbating the problem is the U.K. variant, said Dr. Dr. Adalsteinn Brown, co-chair of the province’s COVID-19 science table on Tuesday.
He said should the variant spread too much in the province, the rate at which our cases double to reduce to about 10 days, from the current rate of 35-40.
"We are at a dangerous point," he said, adding without a significant reduction in contacts, the health system will become overwhelmed.
The Ontario Hospital Association said last week it was preparing for a Team Ontario approach to intensive care, preparing to shift patients in and out of regions depending on capacity.
Premier Doug Ford and Health Minister Christine Elliott said this week the same approach could be used for staff, moving doctors in and out of regions based on each hospital's needs.
There have been less than 3,000 cases in three of the last four days, but the seven-day average remains well above 3,000.
Warner said the memo issued on Wednesday made him very uncomfortable
"It's morally distressing and it's terrible for patients," he told CBC.
In response to the numbers on Tuesday, the province instituted a Stay-At-Home order and issued its second state of emergency during the pandemic.